The main reason I started this blog was to lend a voice to the experience of having a baby after postpartum depression. At that time, my advocacy for families struggling with Postpartum Mood & Anxiety Disorders was in its infancy.
Over the past few years, my experiences, both personal and online, have lent to an understanding that it’s not only moms who experience depression after the birth of a child.
I’ve interviewed dads like Joel Schwartzberg and Jeff Tow who have personally experienced it. I’ve lived with a dad who experienced it. I’ve spoken with experts who have conducted research in the area and also with experts such as Dr. Will Courtenay, who provide counseling and support for men who experience what is properly termed as “Paternal Postnatal Depression.”
Yesterday, The Guardian published a piece by Barbara Ellen entitled, ” ‘Postnatally depressed’ dads? Give me a break.” I read it this morning as yesterday I was on the road. Barely awake and still blinking to bring words into focus, I saw a tweet on my timeline referring to the article. I clicked. It was a response post by the folks over at Mind Hacks. I knew this required more response than I could provide via Twitter. So here I am.
[tweet https://twitter.com/mindhacksblog/status/191478302169501696 align=’center’]
The Guardian has a less than stellar record when it comes to Postnatal Depression stories to begin with so I’m not terribly surprised they allowed something such as this to be posted. More often than not, stories involving PND at The Guardian include gruesome details with no trigger warnings, and they also link to further triggering articles. No resources or further information is ever given.
Let’s begin by examining the definition of postnatal:
post·na·tal (p
st-n
t
l) adj. Of or occurring after birth, especially in the period immediately after birth.
It states “after birth,” yes? It does not state “after giving birth.” Postnatal depression, for most women, is intrinsically linked to childbirth, but according to Ms. Ellen, adoptive parents are also excluded from the experience of Postnatal depression because they fail her test for the qualifications to achieve proper “Postnatal Depression” legitmacy:
“Were hormonal levels tested? Was postpartum bruising measured? How about the emergence of a human head in what – in deference to what might be your leisurely Sunday breakfast – I will refer to as the front-bottom area?”
What about women who had a cesarean section? Given that their child also did not technically emerge from “the front bottom area”, are they also excluded from experiencing Postnatal depression?
Ms. Ellen, in her bashing of men who experience Postnatal Depression, does not just bash them. She completely denigrates any experience of Postnatal Depression. It’s clear she read the research but I wonder if she bothered to even talk to any men who have experienced Paternal Postnatal Depression. Or frankly, if she even cares to, given her obvious feelings on the topic:
“The research from Oxford University is all about new fathers becoming stressed and depressed, their condition triggered by the sleepless nights, strain and the responsibilities of parenthood. I believe the official medical term for this is: “Pissed off, knackered and yearning to be carefree again.” “
The addition of an infant, to any relationship, is a difficult one. There are sleepless nights, there is strain, and there absolutely are responsibilities of parenthood. Some of us fight even darker demons after the birth of a child, regardless of our gender, regardless of how (or even if) we gave birth, and, regardless of our socioeconomic status.
I watched my former spouse fight Paternal Postnatal Depression as I fought my own battles with Postpartum OCD, Depression, and PTSD. His experience is no less valid than my own, and I certainly did not feel as Ms. Ellen states I should have felt,
“…were having to put up with such exhausting narcissists as partners – men incapable of hiding their sulky self-absorption…”
There’s an importance in acknowledging men with depression after the birth of a child. Why? Because men are far more likely than women to complete suicide. They are also more likely to TAKE THEIR FAMILIES WITH THEM.
This is not solely a male v. female issue. This is not men attempting to lay claim to “…a foul, debilitating condition directly related to the physical act of pregnancy and childbirth?” This is a family issue, just as it is with a mom. This is a mental health issue. Men, yes, are capable of experiencing depression. It doesn’t make them any less of a man, it doesn’t mean we suddenly have to contend with “male PND.” It means we should be understanding, accepting, and supportive of fathers, a group who is largely forgotten after the birth of a child and is simply assumed to carry on as if his life has not changed.
Men are more involved in the childbirth experience than ever before. They are in the delivery room, they are staying home to take care of their children, and they are engaging in their children’s lives. Why shouldn’t we acknowledge their struggle? Men experiencing emotion is not new. It’s simply not accepted by society and therefore brushed under the rug.
Let’s stop doing this.
As I told my son, who broke down in tears after Skyping with his Dad, it’s okay for him to cry. Anyone telling him any differently is wrong. It’s okay for a man to cry. It’s possible for a man to be depressed after the birth of a child – it’s not him feeling “pissed off, knackered, or yearning to be carefree.”
Stop giving ignorance a platform, dear media. Just stop.


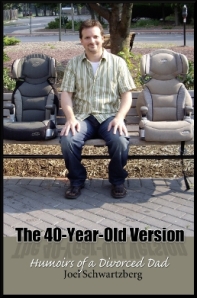 An interview with Joel Schwartzberg, author of The 40 Year old Version: Humoirs of a Divorced Dad, is featured today over at the Postprtum Dads Project. Joel opens up about his depression after the birth of his son, divorce, and how coming to terms with the dad he is helped him feel comfortable in his “dadhood.”
An interview with Joel Schwartzberg, author of The 40 Year old Version: Humoirs of a Divorced Dad, is featured today over at the Postprtum Dads Project. Joel opens up about his depression after the birth of his son, divorce, and how coming to terms with the dad he is helped him feel comfortable in his “dadhood.”