Last night, I had a rather in-depth discussion with Addye over at Butterfly Confessions. We’ve discussed the same topic before and we’re finally doing something about it because we both think there’s not enough out there about this subject. Her blog post went up last night, discussing the role her antenatal depression, postpartum mood disorders, and other mental health struggles have played in her son’s recent diagnosis of being on the autism spectrum. While our children’s diagnoses are different, our story is the same, and it begins with a long hard look at the stinging guilt with which we now carry along our paths of Motherhood.
******************************
It’s taboo, really, more so than admitting you struggled with a Postpartum Mood Disorder. It’s a secret locked in a trunk hidden in a house deep in the woods where no one will find it. It’s the poison-tipped tail of a scorpion, the thing that gets you after the initial reaction of having a scorpion land in front of you. It’s the nagging feeling you get in your throat every damn time you look at your kid and think, even for a brief second, that you did that to them. It’s YOUR fault.
I’ve been there. I still am, sometimes. Not as much as before, but it’s something that I will always carry with me. A small part of my heart will always be tinged with guilt and a depth of sadness I’ll never shake. I’ve learned to accept it instead of fight it, to give it space to just breathe, knowing I’ll never get rid of it as long as I live. Right next to it though, now, is a space that is filled with a peace I’ve worked very hard to achieve – a peace that cancels out that guilt and sadness…as long as the see-saw is working that day, that is.
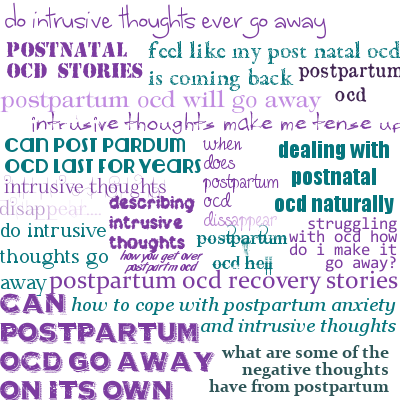
I struggled with Postpartum OCD after the birth of my first daughter. I’ve made no secret of that. I sought help but was shot down by my OB, an integral part of this story. I had to fight on my own to heal. Looking back, I didn’t do a great job at healing. What I excelled at was shoving all of the darkness down and faking it until I felt like I made it. Only by the time I got there, I was pregnant again and my hormones became the scorpion.
They flowed into my pregnancy, along with severe morning sickness. There were days I had to choose between eating or my prenatal vitamin. I often chose eating because I knew the vitamin would make me vomit whereas I might be able to keep the food down. One day, I lived on just one powdered donut. Other days, less. I couldn’t tolerate food for almost four months, if memory serves correctly.
I remember thinking I didn’t need the prenatal vitamin. I’d be okay, baby would be fine. Or so my hormone rattled brain said so. I didn’t want to get up, I would lay on the couch as our oldest, just a little under a year and a half, begged me to play with her. I couldn’t move or I’d vomit. So she learned to play by herself.
The pregnancy progressed, everything seemed fine, I didn’t have Gestational Diabetes again, the baby measured fine, all was good.
Until my baby shower. I went into labor that evening. I was 35wks and 6 days pregnant. (Women with untreated antenatal depression are more likely to go into labor early….or so says the research). At the time, I didn’t relate the two. I just knew I wasn’t full term and contracting. I labored at home until the next morning when we finally saw the doctor. I was dilated enough for them to send me to the hospital. Baby was on her way. Instead of happy, I was nervous. What was wrong? Why was she coming early? We were close enough to full term, really, less than a week away. But still, she was early.
After 42 hours of grueling labor, my daughter was born. She looked perfect. 10 fingers. 10 toes, screaming, a perfect squishable pink human all mine. I made her. As I tried to latch her to nurse, she wouldn’t latch. Just kept screaming. I didn’t know why. I tried for 30 minutes. Then we called the Lactation Consultant. I knew what I was doing, damn it, I had nursed our first for 16 months. Why wouldn’t she latch?
The Lactation Consultant swept her mouth as soon as she got to our room.
That’s when shit got real.
My darling perfect little squishable baby was rushed away from me, the word “cleft palate” left hanging in the air.
There I lay, in a hospital room, epidural still wearing off, all alone, no staff, no husband, nothing to show for almost 2 full days of labor except for the echoing of my heart shattering, insidious voices flooding my head with the phrase, “It’s your fault.”
I did that to her. She grew inside of me, imperfectly.
I lost it that night, brushed my hair for 10 minutes in front of the mirror. Ugly cried on the phone a lot that week, so much so that my ex-husband couldn’t even understand me at several points. In front of nurses. I cried a LOT. This? Wasn’t the way things were supposed to go. Why had I failed?
She was in the NICU for 21 days, undergoing one major surgery for her jaw at just 9 days old. Seeing your 9 day old infant on apparatus breathing FOR her… yeah.. um… yeah. “I did that to her.”
The kicker? The geneticist at the hospital asked me if I took my prenatal vitamins. I lied. I didn’t need any more guilt. I really didn’t. In my fog, I failed a lot.
People told us if we made it through the first year….we’d be scot-free.
They lied.
She’s seven now. Is one of the bubbliest personalities you could ever hope to meet. She’s perfect in every possible way. But she’s struggled so much and her struggles are far from over. Because of me.
She fights for every word she says. It could be worse, I tell myself. She could have so many other issues kids with her same condition have – texture issues, an additional syndrome, etc. Aside from her Pierre Robin Sequence at birth, she’s fine. She has speech therapy, and has had additional surgeries to help with her speech. Before she was 2, she’d been through three times as many surgeries as I have in my entire life.
I did that to her.
What if I’d taken my prenatals? Would she have been born this way? What if I’d fought harder for myself in seeking help for my depression after the birth of her sister?
Intellectually, I KNOW it’s not my fault. But still, the sting is there, long after the scorpion has faded out of sight.
It’s there, just a tinge of it, every time we talk. Every time I have to decipher what she’s said to me based on the context of the words I am able to understand because I still can’t understand every single thing she says. I recently won $200 headphones. They help me immensely in understanding her when we Skype. The ear-buds I had before just weren’t high enough quality to do so. Even now, I have to make her slow down and repeat what she’s said because she’s seven and well, seven year olds get excited.
She will need a lot of orthodontic work. She has the risk of giving birth to a child with similar issues. Kids will tease her because of the way she talks. She was born a fighter without having a say in the matter. While I know this will serve her well later in life, it is something with which I struggle.
Some mothers have Postpartum Depression, Anxiety, PTSD, etc, and they heal, with no adverse affect on their children. But there are those out there who experience issues with their children. And because of what we’ve been through, we draw that line from point PPD to point whatever Alphabet Soup DX with our kids. There’s research to back most of it up. There isn’t research (that I’ve found) to back up PPD related to cleft palate but a “Friend” of mine once tried to draw a line to the type of med I may have taken to my daughter’s cleft palate. Punch.IN.THE.GUT.
Moms like me need a gentle hand. We need to be heard, not dismissed. We don’t need to hear that “It’s not your fault” because in our heads? It is. It always will be no matter how much you tell us that it’s not. It just will be. We need you to stand with us, to be there when we need to scream, cry, vent, and shake our fists at the sky. To understand that our truth is a hard truth and sometimes it will break us but we will rebuild, a constant practice in our lives shattered by this spike of unexpected blow-back from our already complex, shame, and stigma-riddled experiences.
We are women made of glass. Under that glass, yes, we are steel, because we have to be, but on the outside, we are glass and we shatter. We need you to be someone who lets us shatter, someone who helps put us back together and take another step forward as we walk toward processing our new truth.
It’s time for us to come out of the darkness and speak up, to be honest about the role we feel we played in the issues affecting our kids, and to find support, REAL support, not dismissive attitudes, in our search for the light both we and our children need to thrive. We seek out the research drawing the lines from Mom to our kid’s issues, whatever they may be. Sometimes, the line tracing back to Mom is real, worth exploring, and worth understanding. Without it, we’re just left wondering why. I, for one, don’t like hanging out in the middle of nowhere with no answers.
Any answer, even a horrible one, is better than no answer at all.
It’s something. A direction in which we can begin to move forward from, a new beginning from which we can start to walk toward solace. Even if we never reach it, walking toward it is often enough. It has to be, right?