Last week, a friend of mine tagged me in a link on FB to give me a heads up about a NIMH chat this week about Perinatal Mood Disorders. Of course we were looking forward to it and hoping it would be a worthwhile discussion. I nearly missed it on Friday morning (May 16, 2014) thanks to a nasty case of food poisoning which knocked me off my feet for the better part of this week. But, I managed to dive in just 10 minutes into the chat.
It was…….awful.
Stilted.
Non-engaging.
Spouting of facts and just the facts, according to the NIMH. (They managed to screw up a few things. Don’t worry, I’ll go there. Oh, yes, yes I will.)
Self-promotion and only self-promotion. No real response to the powerful Perinatal Mood and Anxiety Disorder Advocates who showed up until we started really pushing back. Even then, their response was still stilted.
Just when it seemed it couldn’t get any worse, the NIMH began repeating tweets from the beginning of the chat instead of answering the flurry of questions coming in from those participating.
If NIMH handed this chat in as a graded project, it would have received an F.
When I asked what was being done to encourage medical professionals to become better educated about PMAD’s, this happened:
Yep.
Congress MANDATED we pay more attention to PMAD’s. In fact, it got shoved in with the ACA. And we all know how well that’s going. After this response, I asked a follow up question asking how that was going – asked for hard numbers. Did I get numbers? Nope. BECAUSE THE ATTENTION MANDATED BY CONGRESS LACKS FUNDING AND THEREFORE ATTENTION.
I’m okay, I’m okay. *deep breath*
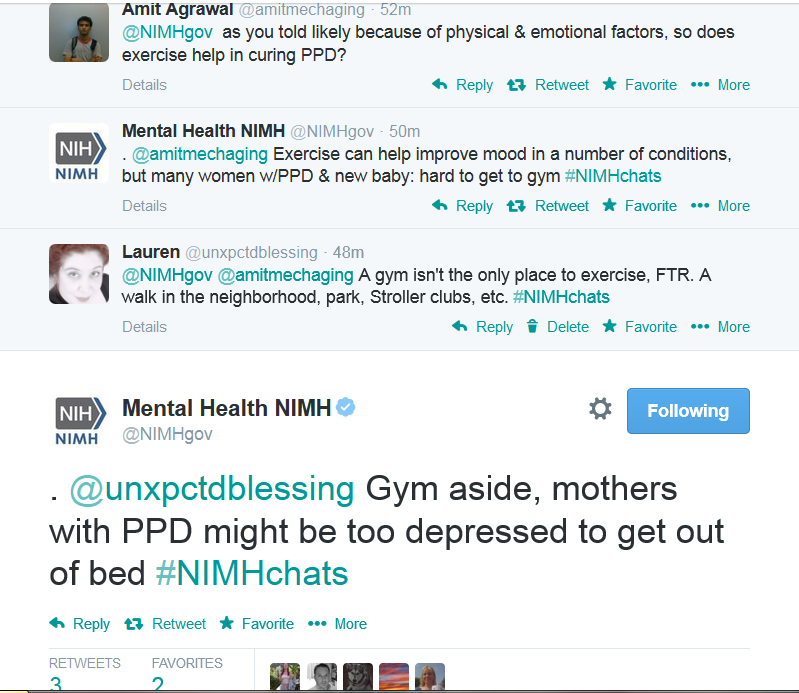
There was also this lovely moment in chat:
I know, right?
Because we ALL got better by staying in bed thanks to depression, right? Right?
Instead of urging moms to get up, move, and care for themselves, the NIMH provides them with excuses to stay in bed and well, suffer. Way to go, NIMH. WAY.TO.GO. *slow claps*
While I realize it is difficult to manage a large scale chat with several participants (something I have done myself, when #PPDChat was very well attended), there is absolutely no excuse for the following to happen during your chat:
1) Blatantly state misinformation/misleading facts about your topic. Particularly if said topic is subject to entrenched stigma and misinformation (which is why you are having the chat to begin with, right? Not because it’s a hot topic and you’re using it to draw people in…)
2) Not engage those who are participating – this is SOCIAL media, y’all. SOCIAL. ENGAGE. Like Jean Luc Picard on the bridge of the Enterprise. Even if you’re just going at impulse speed, ENGAGE for the love of ALL that is..well, you know.
3) Don’t repeat yourself word for word. It lets people know you’re unprepared.
4) Share resources other than your own. (see number 2 about social media).
5) Do NOT TREAT those participating with disdain, contempt, or as if they are idiots. They are attending your event which would be nothing without participants. Respond accordingly unless they are clearly bashing you (which we were not) and if they are bashing you, ignore them before you stoop to the level of responding with disdain.
Things to do during a Twitter chat:
1) Engage. Be Social. Greet people. Be happy and upbeat. SMILE through your keyboard.
2) Be knowledgeable and approachable.
3) Treat everyone as if they are your equal. They are there to learn, not to be kicked. Acknowledge their words, their struggle, their questions with the same respect you expect from them. You know, do unto others as you would have them do unto you.
4) Offer insight through connections and share resources from others in addition to your own. The only answer is not yours. Crowd-source and use the media at hand to enhance your chat.
5) Do your best to make everyone be heard, even if it’s through just RT’ing what they’ve said. Again, I realize this is difficult on a LARGE scale but if you have known experts participating, acknowledge them.
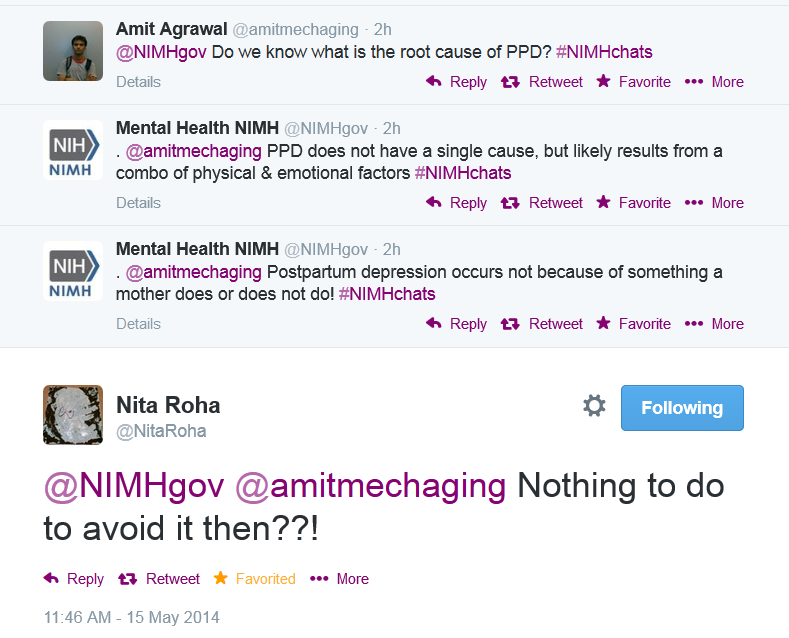
I truly hate when things like this go wrong because there is such a tremendous opportunity for exposure when a government agency holds a chat like this. I want to say I’m surprised at how things went but sadly, I am not. Instead of raising awareness and building hope, NIMH decimated the chat with a lot of tweets about nothing, leaving at least one person (and possibly more) with the idea that there is in fact, nothing a mother can do to prevent a PMAD:
And that, dear friends, is NOT the taste you want to leave in the public’s mouth when discussing PMAD’s. Because there is hope. There is help. We are not alone.
Go to Postpartum Progress to find women who are fighting back.
Or Postpartum Stress Center’s website.
Or find me on Twitter @unxpctdblessing. Or search the hashtag #PPDChat. Message me for the private FB group full of women who KNOW this is hell and yet are fighting back against it with everything they have.
We’re all here for you when you’re ready to reach out for help.
(And THAT is how you end a chat about Postpartum Mood & Anxiety Disorders).
*drops mic and hits publish*